Adults (age 25 or older) are very unlikely to develop eating disorders, (particularly AN, BN and BED) from dieting. Furthermore, purposefully working on weight loss and actually losing weight, when done properly, can cause many physical and psychological benefits. But, before elaborating on these aspects, there are some important details about eating disorders that should be covered first.
The Eating Disorders
Six main feeding and eating disorders are now recognised in diagnostic systems (i.e., DSM-5), which are anorexia nervosa (AN), bulimia nervosa (BN), binge eating disorder (BED), avoidant-restrictive food intake disorder (ARFID), pica, and rumination disorder (these latter three are very different from the other types and will not be covered here as they are not related to the topic at hand).
Eating disorders (EDs) are serious psychiatric conditions and often result in significant psychological and physiological harm. In fact, they (mostly AN), have the highest mortality rate of all mental illnesses. Furthermore, recovery from these disorders is only around 50%; typically lower for AN and the longer the duration of the illness and higher for other types of EDs, particularly if treatment is started early. Interestingly, a fair amount of people will recover without formal treatment (Schaumberg, K., Welch, E., et al 2017). Overall, the outcomes are not great as a fairly high percentage (30-70%) of people with ED’s will often struggle for decades, if not a lifetime. Therefore, it is important to be cautious of doing things that could cause the development of such conditions.
Prevalence of EDs
Collectively, Anorexia nervosa (AN), Bulimia nervosa (BN), Binge-eating disorder (BED), occur in about 4 percent (females 3.8% and males 1.5%) of people. More specifically, AN occurs in about .1 to 2 % of people, BN .1 to 5% and BED ranges from .2 to 4%. If we include the diagnoses of “other specified feeding and eating disorder” (OSFED), then the research is finding a prevalence around 13% (Culbert et al 2015). Although, according to a 2020 in-depth report on the subject, the lifetime occurrence of eating disorders is about 9% (Deloitte Access Economics, 2020). There is a major difference in the occurrence between females and males. Overall, these disorders occur 2-10 times more often in females, so when looking at the ranges, males are usually at the low end and females are often at the high end.
Development of EDs (those based on DSM-5 criteria) typically occurs during puberty and early (10-13) and middle (14-17) adolescence, but can develop during early adulthood (18-25) (Treasure et al 2020; Ward et al 2019) . To be clear, as stated by Ward and colleagues, “Ninety-five percent of first-time cases [of EDs] occurred by age 25 years.” (Ward et al 2019, emphasis added). However, this does not mean adults can’t develop ED’s, they can, it is just very unlikely. Furthermore, adults can still potentially develop unhelpful, although not technically pathological (DSM criteria) relationships with food and dieting. For example, a relatively new classification (not in the DSM), orthorexia, is a situation where there can be an excess focus and rigidity to “eating healthy” which can have negative effects (Strahler, J., & Stark, R. 2020). However, there is still a lot of debate on these classification (Strahler, J., & Stark, R. 2020; Zickgraf et al 2022). Furthermore, there are recommendations to be careful with this classification, such as “We should be sure that the OrNe [Orthorexia nervosa] construct does not over-pathologize an interest in healthy eating; even a strong, focused or restricted interest is not inherently problematic. Obsessive thoughts or compulsive behaviors become problematic when they cause distress or lead to impairment.” (Zickgraf et al 2022).
Risk Factors for Developing EDs
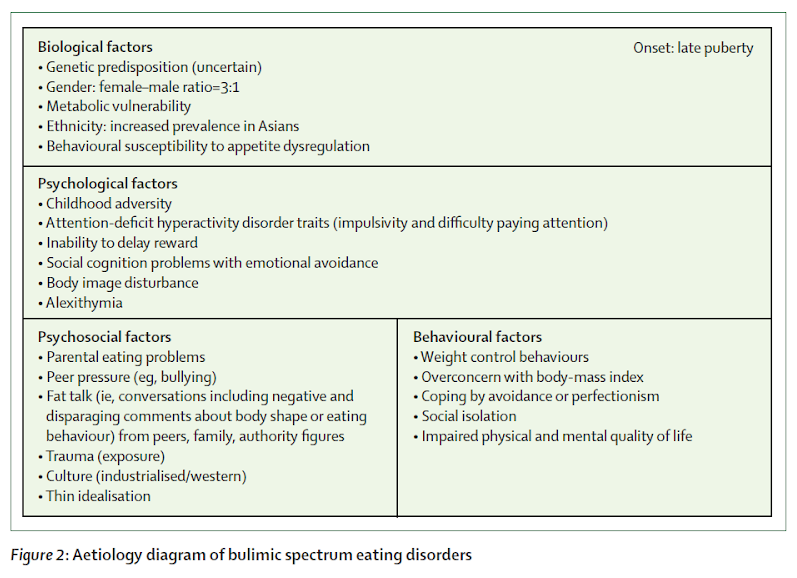
It is clear the cause of EDs is multifactorial, stemming from psychological, physiological and social aspects (Culbert et al 2015; Schaumberg et al 2017; Treasure et al 2020).
The following pictures, Figure 1 and 2, from Treasure and colleagues (2020), are a great overview of the risk factors.
Figure 1

Figure 2
The following is from The Science Behind the Academy for Eating Disorders’ Nine Truths About Eating Disorders (Schaumberg et al 2017)
“7.4 Only a small portion of individuals exposed to environmental risk develop eating disorders
Dieting, drive for thinness, and portion size escalation are widespread in industrialized countries and may represent risk scenarios for the development of eating disorders (Jacobi, Hayward, de Zwaan, Kraemer, & Agras, 2004; Steenhuis & Vermeer, 2009; Striegel-Moore & Bulik, 2007); however, despite nearly ubiquitous exposure, threshold illnesses are disproportionately rare. A current hypothesis is that individuals genetically predisposed to eating disorders are most vulnerable to societal pressures and environmental insults. Eating disorders are “complex traits,” meaning that multiple genetic and environmental factors—each of small to moderate effect— act together to increase risk.”
Some key points from these figures and quote above. First, EDs mostly develop around mid to late puberty. Second, there are many risk factors, with many of them not chosen and likely not modifiable. Third, “weight control behaviors” which can include dieting. is a potential risk factor, but often not the main one. Furthermore, although a risk factor it can also be the result of other issues and therefore not the cause of the eating disorder per se (Stewart, T. M., et al 2022). Fourth and final aspect, not highlighted in the Figures, but discussed in much of the research in this area, is the fact that there is still a major lack of precise understanding of what causes eating disorders and it is likely a combination of factors and not just one thing, like dieting, for example (Culbert et al 2015, Schaumburg et al 2017; Treasure et al 2020). For example, in The Science Behind the Academy for Eating Disorders’ Nine Truths About Eating Disorders, the authors state; “Despite the prevalence and toll that eating disorders exact on society, we lack comprehensive understanding of the etiology [cause] of eating disorders.” (Schaumberg, K., Welch, E., et al 2017, emphasis added)
Risk versus Benefit
This gets us back to dieting, ie. purposefully working on losing weight (body fat). The percentage of people in the US who are overweight or have obesity, is 30.7% and 41.9% (NIH), respectively, so collectively about 70% of the population likely has excess weight (likely fat). Conversely, for all EDs combined it is about 13%. Clearly the percentage of people who struggle with excess weight is exponentially higher than EDs.

This should not diminish the seriousness of EDs and the continued goal to reduce the prevalence of them. However, there is overwhelming evidence there can be major psychological and physiological harm done when we carry excess weight (fat) (Chu et al 2019; Henselmans 2022; Zhang et al 2022). Furthermore, if we are carrying excess weight, and dealing with some health issues, there are many physical and psychological benefits from a reduction in weight (Henselman 2022; Hofer et al 2022; Lasikiewicz et al 2014; Lu et al 2022). These improvements include, but not limited to, blood pressure, lipids, blood sugar, inflammation (which is connected to many chronic conditions) and therefore a reduced risk of developing many of the chronic health conditions prevalent today such as diabetes and cardiovascular disease, just to name a couple. Also, weight loss, if large, has the potential to reverse type 2 diabetes (Brown et al 2022; Taylor R. 2019). Psychologically, weight loss can often bring about improvements in mood and overall cognitive functioning (Fernández-Rodríguez et al 2022; Jones et al 2021; Lasikiewicz et al 2014; Lü et al 2022).
Finally, when dieting is done in an evidence-based manner*, the likelihood it will lead to an eating disorder is extremely unlikely in adults (Chen et al 2021; Dorling et al 2021; National Task Force on the Prevention and Treatment of Obesity 2000; Schaumberg et al 2016; Stewart et al 2022; Wadden et al 2004). In fact, even those with an eating disorder, like BN or BED, can actively work on losing weight (diet) and not exacerbate their condition and typically improve it (Chen et al 2021; F. Q. da Luz et al 2015; Stewart et al 2022). Therefore, if an adult, particularly without an eating disorder, has excess weight (body fat), purposely dieting to lose weight is not tantamount to playing Russian Roulette. Nothing is risk free. However, when comparing the risk of excess weight and the risk of developing eating disorders from dieting, it seems there should be little concern about dieting to lose weight*. But, if there are any concerns a person has an ED or seems to be developing behaviors that are concerning, they should be strongly encouraged to seek advice from a medical/behavioral expert.
*Evidence-based methods are a bit outside the focus of this piece. However, as it is very important, a brief overview seems warranted. The use of the following approaches is likely to lead to greater weight loss and maintenance, as well as, and as important, minimizing/avoiding psychological harm. These helpful methods come from Acceptance and Commitment Theory, Self-Determination Theory; Self-Compassion, Cognitive Behavioral Theory and Motivational Interviewing (Armonstrong et al 2011; Bider et al 2019; Brewer et al 2018; Forman et al 2015; Haynos et al 2016; Jacob et al 2018; Mantzios et al 2017; Palascha et al 2015; Teixeira et al 2012; Thøgersen-Ntoumani et al 2021; Zhang et al 2018) . The overarching goals of these approaches is to foster greater self-compassion and less blame and shame. Additionally, developing more mental flexibility to deal better with all types of thoughts and emotions as well as increase feelings of autonomy and self-efficacy and finally to underpin all goals/behaviors with a clear understanding of personal values. Not to mention, also addressing other important aspects such as physical activity, sleep, and stress. It is these, and other evidence-based strategies, that significantly increase the likelihood of success (reach and maintain a healthy weight) as well as substantially reduce/avoid the risk of harm.
References
Armstrong, M. J., Mottershead, T. A., Ronksley, P. E., Sigal, R. J., Campbell, T. S., & Hemmelgarn, B. R. (2011). Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obesity reviews : an official journal of the International Association for the Study of Obesity, 12(9), 709–723. https://doi.org/10.1111/j.1467-789X.2011.00892.x
Barthels, F., Barrada, J. R., & Roncero, M. (2019). Orthorexia nervosa and healthy orthorexia as new eating styles. PloS one, 14(7), e0219609. https://doi.org/10.1371/journal.pone.0219609
Berg, A. C., Johnson, K. et al (2018). Flexible Eating Behavior Predicts Greater Weight Loss Following a Diet and Exercise Intervention in Older Women. Journal of nutrition in gerontology and geriatrics, 37(1), 14–29. https://doi.org/10.1080/21551197.2018.1435433
Biber, D. D., & Ellis, R. (2019). The effect of self-compassion on the self-regulation of health behaviors: A systematic review. Journal of health psychology, 24(14), 2060–2071. https://doi.org/10.1177/1359105317713361
Brewer, J. A., Ruf, A., Beccia, A. L., Essien, G. I., Finn, L. M., van Lutterveld, R., & Mason, A. E. (2018). Can Mindfulness Address Maladaptive Eating Behaviors? Why Traditional Diet Plans Fail and How New Mechanistic Insights May Lead to Novel Interventions. Frontiers in psychology, 9, 1418. https://doi.org/10.3389/fpsyg.2018.01418
Brown, A., McArdle, P., et al(2022). Dietary strategies for remission of type 2 diabetes: A narrative review. Journal of human nutrition and dietetics : the official journal of the British Dietetic Association, 35(1), 165–178. https://doi.org/10.1111/jhn.12938
CDC. (2022). Adult Obesity Facts. https://www.cdc.gov/obesity/data/adult.html
Cena, H., Barthels, F., et al (2019). Definition and diagnostic criteria for orthorexia nervosa: a narrative review of the literature. Eating and weight disorders : EWD, 24(2), 209–246. https://doi.org/10.1007/s40519-018-0606-y
Chen, J. Y., Singh, S., & Lowe, M. R. (2021). The food restriction wars: Proposed resolution of a primary battle. Physiology & behavior, 240, 113530. https://doi.org/10.1016/j.physbeh.2021.113530
Chu, D. T., Minh Nguyet, N. T., et al (2019). An update on obesity: Mental consequences and psychological interventions. Diabetes & metabolic syndrome, 13(1), 155–160. https://doi.org/10.1016/j.dsx.2018.07.015
Culbert, K. M., Racine, S. E., & Klump, K. L. (2015). Research Review: What we have learned about the causes of eating disorders – a synthesis of sociocultural, psychological, and biological research. Journal of child psychology and psychiatry, and allied disciplines, 56(11), 1141–1164. https://doi.org/10.1111/jcpp.12441
Deloitte Access Economics. (2020). The Social and Economic Cost of Eating Disorders in the United States of America: A Report for the Strategic Training Initiative for the Prevention of Eating Disorders and the Academy for Eating Disorders. June 2020. Available at: https://www.hsph.harvard.edu/striped/report-economic-costs-of-eating-disorders/
Dorling, J. L., van Vliet, S., et al (2021). Effects of caloric restriction on human physiological, psychological, and behavioral outcomes: highlights from CALERIE phase 2. Nutrition reviews, 79(1), 98–113. https://doi.org/10.1093/nutrit/nuaa085
F. Q. da Luz,P. Hay,A. et al (2015). Does severe dietary energy restriction increase binge eating in overweight or obese individuals? A systematic review. Obesity Reviews, 16(8); 652-665
Fernández-Rodríguez, R., Martínez-Vizcaíno, et al (2022). Does intermittent fasting impact mental disorders? A systematic review with meta-analysis. Critical reviews in food science and nutrition, 1–16. Advance online publication. https://doi.org/10.1080/10408398.2022.2088687
Forman, E. M., & Butryn, M. L. (2015). A new look at the science of weight control: how acceptance and commitment strategies can address the challenge of self-regulation. Appetite, 84, 171–180. https://doi.org/10.1016/j.appet.2014.10.004
Haynos, A. et al (2016). Mindfulness and Acceptance for Treating Eating Disorders and Weight Concerns: Evidence-Based Intervention. Context Press
Henselmans, M. (2022). What’s a healthy body fat percentage? Retrieved from https://mennohenselmans.com/what-is-a-healthy-body-fat-percentage/
Hofer, S. J., Carmona-Gutierrez, D., Mueller, M. I., & Madeo, F. (2022). The ups and downs of caloric restriction and fasting: from molecular effects to clinical application. EMBO molecular medicine, 14(1), e14418. https://doi.org/10.15252/emmm.202114418
Jacob, A., Moullec, G., Lavoie, K. L., Laurin, C., Cowan, T., Tisshaw, C., Kazazian, C., Raddatz, C., & Bacon, S. L. (2018). Impact of cognitive-behavioral interventions on weight loss and psychological outcomes: A meta-analysis. Health psychology : official journal of the Division of Health Psychology, American Psychological Association, 37(5), 417–432. https://doi.org/10.1037/hea0000576
Jones, R. A., Lawlor, E. R., et al. (2021). The impact of adult behavioural weight management interventions on mental health: A systematic review and meta-analysis. Obesity reviews : an official journal of the International Association for the Study of Obesity, 22(4), e13150. https://doi.org/10.1111/obr.13150
Lasikiewicz, N., Myrissa, K., Hoyland, A., & Lawton, C. L. (2014). Psychological benefits of weight loss following behavioural and/or dietary weight loss interventions. A systematic research review. Appetite, 72, 123–137. https://doi.org/10.1016/j.appet.2013.09.017
Lü, W., Yu, T., & Kuang, W. (2022). Effects of dietary restriction on cognitive function: a systematic review and meta-analysis. Nutritional neuroscience, 1–11. Advance online publication. https://doi.org/10.1080/1028415X.2022.2068876
Mantzios, M., & Egan, H. H. (2017). On the Role of Self-compassion and Self-kindness in Weight Regulation and Health Behavior Change. Frontiers in psychology, 8, 229. https://doi.org/10.3389/fpsyg.2017.00229
National Task Force on the Prevention and Treatment of Obesity. (2000). Dieting and the development of eating disorders in overweight and obese adults. Archives of internal medicine, 160(17), 2581–2589. https://doi.org/10.1001/archinte.160.17.2581
NIH. (2021). Overweight & Obesity Statistics, https://www.niddk.nih.gov/health-information/health-statistics/overweight-obesity
Palascha, A., van Kleef, E., & van Trijp, H. C. (2015). How does thinking in Black and White terms relate to eating behavior and weight regain?. Journal of health psychology, 20(5), 638–648. https://doi.org/10.1177/1359105315573440
Schaumberg, K., Anderson, D. A., et al (2016). Dietary restraint: what’s the harm? A review of the relationship between dietary restraint, weight trajectory and the development of eating pathology. Clinical obesity, 6(2), 89–100. https://doi.org/10.1111/cob.12134
Schaumberg, K., Welch, E., et al (2017). The Science Behind the Academy for Eating Disorders’ Nine Truths About Eating Disorders. European eating disorders review : the journal of the Eating Disorders Association, 25(6), 432–450. https://doi.org/10.1002/erv.2553
Stewart, T. M., Martin, C. K., & Williamson, D. A. (2022). The Complicated Relationship between Dieting, Dietary Restraint, Caloric Restriction, and Eating Disorders: Is a Shift in Public Health Messaging Warranted?. International journal of environmental research and public health, 19(1), 491. https://doi.org/10.3390/ijerph19010491
Stewart, T. M., Williamson, D. A., & White, M. A. (2002). Rigid vs. flexible dieting: association with eating disorder symptoms in nonobese women. Appetite, 38(1), 39–44. https://doi.org/10.1006/appe.2001.0445
Strahler, J., & Stark, R. (2020). Perspective: Classifying Orthorexia Nervosa as a New Mental Illness-Much Discussion, Little Evidence. Advances in nutrition (Bethesda, Md.), 11(4), 784–789. https://doi.org/10.1093/advances/nmaa012
Stutts L. A. (2020). It’s complicated: The relationship between orthorexia and weight/shape concerns, eating behaviors, and mood. Eating behaviors, 39, 101444. https://doi.org/10.1016/j.eatbeh.2020.101444
Taylor R. (2019). Calorie restriction for long-term remission of type 2 diabetes. Clinical medicine (London, England), 19(1), 37–42. https://doi.org/10.7861/clinmedicine.19-1-37
Teixeira, P. J., Silva, M. N., Mata, J., Palmeira, A. L., & Markland, D. (2012). Motivation, self-determination, and long-term weight control. The international journal of behavioral nutrition and physical activity, 9, 22. https://doi.org/10.1186/1479-5868-9-22
Thøgersen-Ntoumani, C., Dodos, L. A., Stenling, A., & Ntoumanis, N. (2021). Does self-compassion help to deal with dietary lapses among overweight and obese adults who pursue weight-loss goals?. British journal of health psychology, 26(3), 767–788. https://doi.org/10.1111/bjhp.12499
Treasure, J., Duarte, T. A., & Schmidt, U. (2020). Eating disorders. Lancet (London, England), 395(10227), 899–911. https://doi.org/10.1016/S0140-6736(20)30059-3
Wadden, T. A., Foster, G. D., et al (2004). Dieting and the development of eating disorders in obese women: results of a randomized controlled trial. The American journal of clinical nutrition, 80(3), 560–568. https://doi.org/10.1093/ajcn/80.3.560
Ward, Z. J., Rodriguez, et al (2019). Estimation of Eating Disorders Prevalence by Age and Associations With Mortality in a Simulated Nationally Representative US Cohort. JAMA network open, 2(10), e1912925. https://doi.org/10.1001/jamanetworkopen.2019.12925
Williamson, D. A.,et al & Pennington CALERIE Team (2008). Is caloric restriction associated with development of eating-disorder symptoms? Results from the CALERIE trial. Health psychology : official journal of the Division of Health Psychology, American Psychological Association, 27(1S), S32–S42. https://doi.org/10.1037/0278-6133.27.1.S32
Zhang, Q., Jin, K., Chen, B., Liu, R., Cheng, S., Zhang, Y., & Lu, J. (2022). Overnutrition Induced Cognitive Impairment: Insulin Resistance, Gut-Brain Axis, and Neuroinflammation. Frontiers in neuroscience, 16, 884579. https://doi.org/10.3389/fnins.2022.884579
Zhang, C. Q., Leeming, E., Smith, P., Chung, P. K., Hagger, M. S., & Hayes, S. C. (2018). Acceptance and Commitment Therapy for Health Behavior Change: A Contextually-Driven Approach. Frontiers in psychology, 8, 2350. https://doi.org/10.3389/fpsyg.2017.02350
Zickgraf, H. F., & Barrada, J. R. (2022). Orthorexia nervosa vs. healthy orthorexia: relationships with disordered eating, eating behavior, and healthy lifestyle choices. Eating and weight disorders : EWD, 27(4), 1313–1325. https://doi.org/10.1007/s40519-021-01263-9
